
Living your best life necessitates a life in balance.
In Part 1 of our “Life in BALANCE” research update Dr. Farley described how the process of balance control is complex and infers an equilibrium across multiple physiological systems (i.e., sensory, musculoskeletal, neuromuscular, cognitive) with environmental and task factors.1-3. Unfortunately for all of us, dysfunction in any of these systems can interfere with our ability to remain upright and steady.4 But, for persons with Parkinson disease (PWP), the motor and nonmotor symptoms of Parkinson disease (PD) and the side effects of dopaminergic medications and deep brain stimulation1-5 can further contribute to dysfunction in balance control and lead to negative psychological effects (e.g., fear, anxiety) and reduced mobility (e.g., gait, everyday activities) and participation in life (e.g., withdraw from doing the things you love doing).1-4,6
Our Balance Guided Plans
are available to begin today!
50% off for 3 months!
Enter SUMMER2021 at Checkout
Receive 50% off your subscription for 3 months.
We want you to keep active for summer.
Take us with you!
We offer Live and On-Demand.
We'll see you soon!
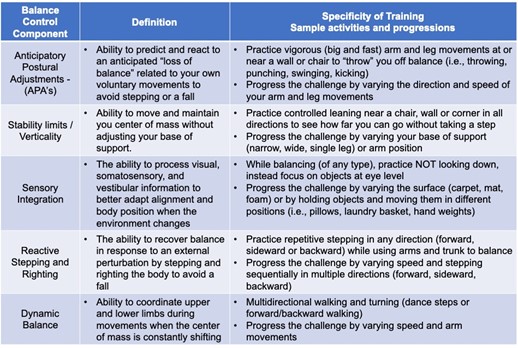
To understand how the symptoms of PD impact balance control, researchers have developed conceptual frameworks to describe the components underlying balance control in healthy populations. These frameworks allow therapists to perform assessments to identify dysfunctional balance components in PwP who are at risk for falls. The same framework also provides a theoretical foundation for developing PD-specific balance interventions. I have modified those frameworks for simplification and to help with translating the information from research into our PWR!Gym programs in Table 1 below. For each balance control component, there is a definition and an example of an activity targeting that balance component with a few ideas for how to progress the challenge over time. These sample activities and progressions are representative of what you will experience in this months’ prerecorded or live classes.
Table 1. Framework for understanding and integrating PD-specific balance components into PWR!Gym therapy and group exercise programming (modified from references4-6).
These types of highly specific and progressively challenging interventions summarized in Table 1, have been shown to improve gait, balance, and function out to 6 months7-10 and to create structural changes in the brain in PwP.11 In addition, total physical activity (i.e., steps per day) and the number of bouts of moderate physical activity per day (i.e., brisk walking) also increased6 suggesting this type of balance training may reduce sedentary behavior. This has implications for health, quality of life, decreased risk of noncommunicable disease or all-cause mortality, and may represent a physical activity threshold to maintain functional independence! More recently, studies have shown that when those same research protocols are translated into real-world clinics the result are similarly effective.8-10 In fact, results are even longer-lasting (i.e., out to 12 months)12-13 when interventions include indoor and outdoor practice and when practice can be sustained over time.
One thing is for sure - the most effective balance interventions incorporate multiple balance control components and progress the physical and cognitive challenge over time. 7-10,12-13
If all this sounds complicated – it is!
That is why we are here…..we have put it all together for you…..mixing all the components into our pre-recorded and live classes this month.
Not too much, not too little of any one thing.
Are you ready to be proactive and put off or improve the balance control challenges in your life? Are you ready for better mobility and the ability to participate in exercise and community?
Ready to get started? Not sure what to do?
Schedule an appointment with one of our PWR!Gym Therapists to assess your balance control and provide you with a personalized plan.
Working 1:1 with a physical therapist is the most efficient and effective way to “retrain” balance, group exercise is the most effective way to “sustain” the gains from therapy! Guess what? At the PWR!Gym, we can give you access to both – intensive bouts of PD-specialized rehabilitation and group exercise training for life.
Come join us at the PWR! Virtual Experience and live YOUR “Life in Balance.”
Synopsis or Bottom Line
Synopsis or Bottom Line: Of all the types of exercise people with PD can do, balance training rates up there as one of the most important. Not only does better balance generalize to better gait and everyday function, but it also results in increased physical activity (with lower risk of falls). That means you get more benefit for your time and effort and are more likely to keep doing things you like to do. You just need to be sure that after a balance training program you keep practicing your skills at home and in the community and get a balance assessment with your physical therapist every 6-12 months to optimize your balance control program.
Come join us at the PWR! Virtual Experience and live YOUR “Life in Balance.”
Still not sure if you need balance training? Increase your awareness by reflecting on these “red flags” below that put you at a high risk for balance dysfunction and falls.
- Fallen in the last 12 months (A previous fall is predictive of a second fall)
- Defined as: moving downward and coming to rest on the ground, floor, or lower level; even if you have landed on your hands
- Stumbled (no obvious reason)
- Tripped (over object or changes in environment)
- Unsteadiness when walking (beyond klutziness!)
- Bumping into tables or walls (especially when turning or carrying something)
- Furniture cruise
- Unexplained bruising
- Lightheadedness
- Veering left or right when walking
- Struggling to walk in a dark room
- Pain that interferes with movement
- Fear of falling or reduced balance confidence
- Slow, shuffling walking
- Loss of flexibility in ankles, knees, hips and trunk
- Stopped participating in physical activity that you enjoy

Our goal is to make sure you’re always empowered and informed.
We offer handouts, downloads, research updates, Wellness Series talks, retreats with knowledgeable speakers, in-person and virtual wellness consultations, and in-person physical therapy visits. We are here for our PWR! Members every step of the way.
We’re excited to have you join us!
References
- King LA, Horak FB. Delaying Mobility Disability in People With Parkinson Disease Using a Sensorimotor Agility Exercise Program. Phys Ther. 2009;89(4):384-393. doi:10.2522/ptj.20080214
- Schoneburg B, Mancini M, Horak F, Nutt JG. Framework for understanding balance dysfunction in Parkinson’s disease. Mov Disord. 2013;28(11):1474-1482. doi:10.1002/mds.25613.
- Conradsson D, Löfgren N, Ståhle A, Hagströmer M, Franzén E. A novel conceptual framework for balance training in Parkinson’s disease-study protocol for a randomised controlled trial. BMC Neurol. 2012;12(1):111. doi:10.1186/1471-2377-12-111
- Fasano A, Canning CG, Hausdorff JM, Lord S, Rochester L. Falls in Parkinson’s disease: A complex and evolving picture. Mov Disord. 2017;32(11):1524-1536. doi:10.1002/mds.27195
- Debû B, De Oliveira Godeiro C, Lino JC, Moro E. Managing Gait, Balance, and Posture in Parkinson’s Disease. Curr Neurol Neurosci reports. 2018;18(23). doi:10.1007/s11910-018-0828-4
- Nero H, Franzén E, Ståhle A, Benka Wallén M, Hagströmer M. Long-Term Effects of Balance Training on Habitual Physical Activity in Older Adults with Parkinson’s Disease. Parkinsons Dis. 2019;2019:1-9. doi:10.1155/2019/8769141
- Conradsson D, Löfgren N, Nero H, et al. The Effects of Highly Challenging Balance Training in Elderly With Parkinson’s Disease. Neurorehabil Neural Repair. 2015;29(9):827-836. doi:10.1177/1545968314567150
- Leavy B, Kwak L, Hagströmer M, Franzén E. Evaluation and implementation of highly challenging balance training in clinical practice for people with Parkinson’s disease: Protocol for the HiBalance effectiveness-implementation trial. BMC Neurol. 2017;17(1):1-9. doi:10.1186/s12883-017-0809-2
- Leavy B, Joseph C, Löfgren N, Johansson H, Hagströmer M, Franzén E. Outcome Evaluation of Highly Challenging Balance Training for People With Parkinson Disease: A Multicenter Effectiveness-Implementation Study. J Neurol Phys Ther. 2020;44(1):15-22. doi:10.1097/NPT.0000000000000298
- Wong-Yu IS, Mak MK. Task- and Context-Specific Balance Training Program Enhances Dynamic Balance and Functional Performance in Parkinsonian Nonfallers: A Randomized Controlled Trial with Six-Month Follow-Up. Arch Phys Med Rehabil. 2015;96(12):2103-2111. doi:10.1016/j.apmr.2015.08.409
- Sehm B, Taubert M, Conde V, et al. Structural brain plasticity in Parkinson’s disease induced by balance training. Neurobiol Aging. 2014;35(1):232-239. doi:10.1016/j.neurobiolaging.2013.06.021
- Wallén MB, Hagströmer M, Conradsson D, Sorjonen K, Franzén E. Long-term effects of highly challenging balance training in Parkinson’s disease—a randomized controlled trial. Clin Rehabil. 2018;32(11):026921551878433. doi:10.1177/0269215518784338
- Wong-Yu ISK, Mak MKY. Multi-dimensional balance training programme improves balance and gait performance in people with Parkinson’s disease: A pragmatic randomized controlled trial with 12-month follow-up. Park Relat Disord. 2015;21(6):615-621. doi:10.1016/j.parkreldis.2015.03.022
Dr. Becky Farley About the Author
If you ask her, Dr. Becky Farley will tell you that working with her first client with Parkinson’s almost 20 years ago changed her life and her career, and since then she hasn't stopped changing lives of those living with Parkinson's, in Arizona and the rest of the world. In 2010, she established the PWR!Gym in Tucson and has been offering people with Parkinson disease the PD-specific physical therapy, group exercise, and social engagement they need to get better and stay better. Globally, Dr. Farley supports PWR!’s mission of making cutting-edge PD-specific "exercise as medicine” available to the 10 million people living with PD worldwide, by training healthcare and fitness professionals in the PWR!Moves and the PWR!4Life model (and she’s trained over 6000 professionals since she started in 2010!).
When she’s home in Arizona, you’ll find Becky working on PD-specific exercise at the PWR!Gym as well as leading our annual exercise intensive PWR! Retreats. When she’s on the road, she’s either teaching our PWR!Moves workshops or giving talks at conferences, community organizations, and healthcare networks across the US and world.
When she isn’t working, you can find her working out, walking the dog, and gardening. To learn even more about Dr. Farley, visit our team page.

You can find Dr. Farley at: