
Let’s have FUN with Function - “Make Function Exercise”
Our Function Guided Plans
are available to begin today!
I am excited to talk to you about the “Function” guided plan and why function is the PWR!Gym’s primary focus for group exercise and rehabilitation! Ever since my NIH funded research established the importance of intensive whole-body amplitude training as a 4-week rehabilitation protocol (LSVT BIG ®) for improving function in persons with Parkinson disease, I wanted to do more to get at the heart of the mobility and functionality problems in persons with Parkinson disease (PD)1-4. I knew an approach with a singular attentional focus on amplitude (for the symptom of bradykinesia) was not enough4-5. Instead, a more comprehensive approach was needed to target all the motor and cognitive symptoms of PD that contribute to the loss of functional mobility2-4,6-8 (and see the definition in Figure 1 below). Then we need to make sure people continue to practice those same high quality functional movements after rehabilitation at home and in community9-10!
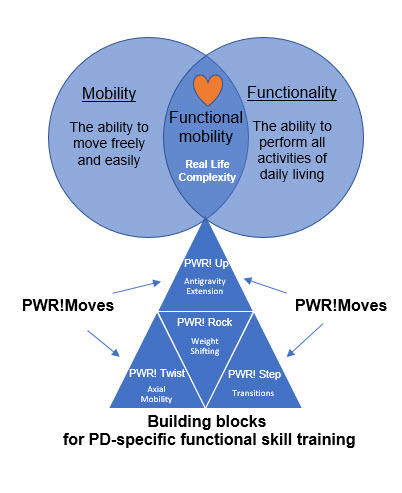
Functional Mobility Defined
The ability to move freely (mobility) and to perform all your activities of daily living (ADL’s) (functionality) independently and safely in complex and changing environments at home, work and in the community (functional mobility in the real world).
Why retraining and sustaining functional mobility is the “heart” of what we do.
The loss of functional mobility is a global disease-related feature of Parkinson disease (PD) and a major cause of disability6-8, 11. In Figure 1, the pyramid at the bottom highlights the motor control skills that deteriorate in PD and contribute to the loss of functional mobility (i.e., antigravity extension, weight shifting, axial mobility, transitions)4. These skills are initially learned in development. Once these building blocks are learned, you usually never think about them. They just occur spontaneously when needed. These building blocks of function are necessary for ALL physical activity. If they deteriorate, not only will your function deteriorate, but so will your fitness (endurance, strength, balance, agility, and flexibility). That is why we start with the building blocks of function (i.e., PWR!Moves). They are the PD-specific skills you need to train and sustain function and fitness - in order to put off the motor and cognitive decline – and continue to do the things you love to do.
Our rehab and group exercise programs have shared goals to “preserve function.”
We want you to have functional mobility.
Whether you are participating in rehabilitation or group exercise, we start by practicing the basic PWR!Moves in isolation for flexibility and whole-body “vigor” and strength – to get you ready for more skilled “task specific” or “fitness-specific” practice, respectively2-4,8,12-14. In rehabilitation, your therapists will focus on a personalized plan of care to target specific mobility or functional activities related to how your motor and nonmotor symptoms are interfering with your “real world” functional mobility6-8. In group exercise classes, your instructors will integrate the PWR!Moves into fitness programming (strength, agility, balance, flexibility) and make function exercise12-14!
Cycling back and forth from rehab to community exercise and back will help train and sustain your functional mobility and increase your overall physical activity to fully engage in life!
In part 2, learn more about the specific guided plan on function.
Functional Mobility can be as basic, but as important as standing to sitting & standing again.
"I can still sit to stand the same amount per minute as I could when I was diagnosed with Parkinson's 5 years ago. It is my goal to maintain my ability to sit to stand. And I do it with PWR!Moves " - PWR!Gym Member

Ready to get started? Not sure what to do?
Schedule an appointment with the PWR!Gym to assess your balance control and provide you with a personalized plan.
Working 1:1 with a therapist is the most efficient and effective way to “retrain” balance, group exercise is the most effective way to “sustain” the gains from therapy! Guess what? At the PWR!Gym, we can give you access to both – intensive bouts of PD-specialized rehabilitation and group exercise training for life.
Come join us at the PWR! Virtual Experience

Our goal is to make sure you’re always empowered and informed.
We offer handouts, downloads, research updates, Wellness Series talks, retreats with knowledgeable speakers, in-person and virtual wellness consultations, and in-person physical therapy visits. We are here for our PWR! Members every step of the way.
We’re excited to have you join us!
References
- Farley BG, Koshland GF. Training BIG to move faster: the application of the speed-amplitude relation as a rehabilitation strategy for people with Parkinson’s disease. Exp Brain Res. 2005;167(3):462-467. doi:10.1007/s00221-005-0179-7
- Perry SIB, Nelissen PM, Siemonsma P, Lucas C. The effect of functional-task training on activities of daily living for people with Parkinson`s disease, a systematic review with meta-analysis. Complement Ther Med. 2019;42:312-321. doi:10.1016/j.ctim.2018.12.008
- Radder DLM, Lígia Silva de Lima A, Domingos J, et al. Physiotherapy in Parkinson’s Disease: A Meta-Analysis of Present Treatment Modalities. Neurorehabil Neural Repair. 2020;34(10):871-880. doi:10.1177/1545968320952799
- King LA, Horak FB. Delaying Mobility Disability in People With Parkinson Disease Using a Sensorimotor Agility Exercise Program. Phys Ther. 2009;89(4):384-393. doi:10.2522/ptj.20080214
- Farley BG, Fox CM, Ramig LO, McFarland DH. Intensive amplitude-specific therapeutic approaches for Parkinson’s disease: Toward a neuroplasticity-principled rehabilitation model. Top Geriatr Rehabil. 2008;24(2):99-114. doi:10.1097/01.TGR.0000318898.87690.0d
- Vojciechowski AS, Gianello T, Zotz G, Paula A, Loureiro C, Israel VL. The International Classification of Functioning , Disability and Health as Applied to Parkinson ’ s Disease : A Literature Review. 2016;(May):29-40. doi:10.4236/apd.2016.52005
- Ferrazzoli D, Ortelli P, Madeo G, Giladi N, Petzinger GM, Frazzitta G. Basal ganglia and beyond: The interplay between motor and cognitive aspects in Parkinson’s disease rehabilitation. Neurosci Biobehav Rev. 2018;90:294-308. doi:10.1016/j.neubiorev.2018.05.007
- Bouça-Machado R, Maetzler W, Ferreira JJ. What is Functional Mobility Applied to Parkinson’s Disease? J Parkinsons Dis. 2018;8(1):121-130. doi:10.3233/JPD-171233
- Borchers EE, McIsaac TL, Bazan-Wigle JK, Elkins AJ, Bay RC, Farley BG. A physical therapy decision-making tool for stratifying persons with Parkinson’s disease into community exercise classes. Neurodegener Dis Manag. 2019;9(6):nmt-2019-0019. doi:10.2217/nmt-2019-0019
- Mak MK, Wong-Yu IS, Shen X, Chung CL. Long-term effects of exercise and physical therapy in people with Parkinson disease. Nat Rev Neurol. 2017;13(11):689-703. doi:10.1038/nrneurol.2017.128
- Sacheli MA, Neva JL, Lakhani B, et al. Exercise increases caudate dopamine release and ventral striatal activation in Parkinson’s disease. Mov Disord. 2019;34(12):1891-1900. doi:10.1002/mds.27865
- Bouça-Machado R, Venturelli M, Tinazzi M, Schena F, Ferreira JJ. Treating Patients Like Athletes: Sports Science Applied to Parkinson’s Disease. Front Neurol. 2020;11:228. doi:10.3389/fneur.2020.00228
- Prodoehl J, Rafferty MR, David FJ, et al. Two-year exercise program improves physical function in Parkinson’s disease: The PRET-PD randomized clinical trial. Neurorehabil Neural Repair. 2015;29(2):112-122. doi:10.1177/1545968314539732
- Van Puymbroeck M, Walter A, Hawkins BL, et al. Functional Improvements in Parkinson’s Disease Following a Randomized Trial of Yoga. Evidence-Based Complement Altern Med. 2018;2018:1-8. doi:10.1155/2018/8516351
- Durstine, J L, Geoffrey E. Moore, and Patricia L. Painter (eds). ACSM’s Exercise Management for Persons with Chronic Diseases and Disabilities 4th Edition Print. Human Kinetics, Champaign, IL, 2016.
Dr. Becky Farley About the Author
If you ask her, Dr. Becky Farley will tell you that working with her first client with Parkinson’s almost 20 years ago changed her life and her career, and since then she hasn't stopped changing lives of those living with Parkinson's, in Arizona and the rest of the world. In 2010, she established the PWR!Gym in Tucson and has been offering people with Parkinson disease the PD-specific physical therapy, group exercise, and social engagement they need to get better and stay better. Globally, Dr. Farley supports PWR!’s mission of making cutting-edge PD-specific "exercise as medicine” available to the 10 million people living with PD worldwide, by training healthcare and fitness professionals in the PWR!Moves and the PWR!4Life model (and she’s trained over 6000 professionals since she started in 2010!).
When she’s home in Arizona, you’ll find Becky working on PD-specific exercise at the PWR!Gym as well as leading our annual exercise intensive PWR! Retreats. When she’s on the road, she’s either teaching our PWR!Moves workshops or giving talks at conferences, community organizations, and healthcare networks across the US and world.
When she isn’t working, you can find her working out, walking the dog, and gardening. To learn even more about Dr. Farley, visit our team page.

You can find Dr. Farley at: